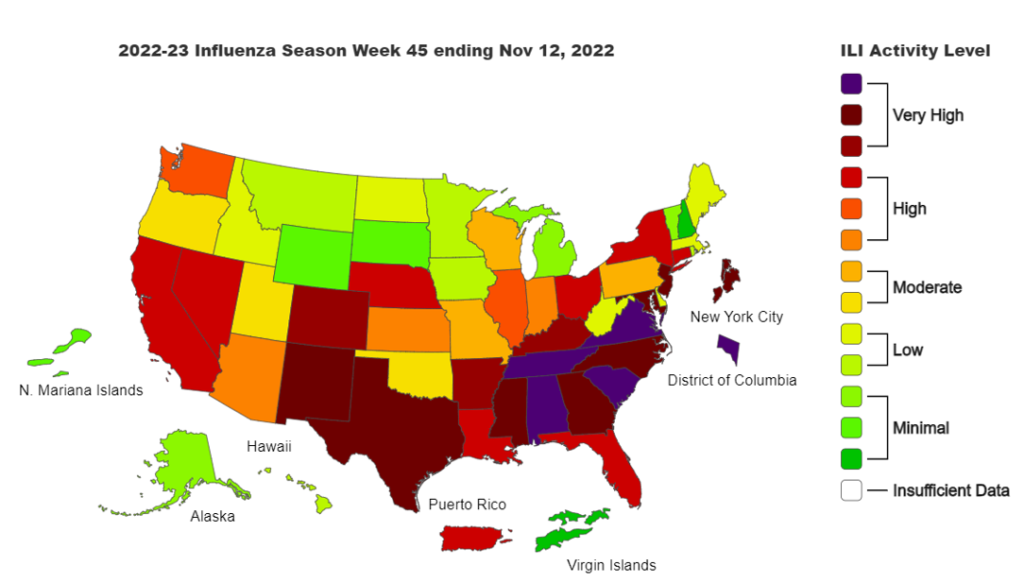
Influenza is continuing to spread across the U.S. and has been declared an epidemic in Canada, and, like COVID, it’s not just a single variant that is spreading. As detailed by CDC, there are four types of influenza viruses: A, B, C and D:
- A and B viruses cause seasonal epidemics (i.e., flu season) almost every winter in the U.S., but A viruses are the only ones known to cause global pandemics.
- C virus infections generally cause mild illness and are not thought to cause human epidemics.
- D viruses primarily affect cattle and are not known to infect or cause illness in people.
The CDC graphic shows the two types of influenza viruses (A and B) that cause most human illness. Each is further divided into subtypes (A)/lineages (B), then into clades and sub-clades (or groups and sub-groups), as shown in the examples in the graphic.
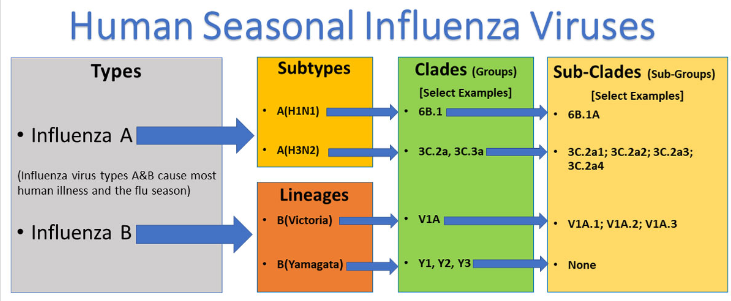
To further explain: The current subtypes of A that routinely circulate in people include A(H1N1) and A(H3N2). Flu viruses have hemagglutinin (H) and neuraminidase (N) surface proteins which act as antigens: molecular structures on the surface that are recognized by the immune system and can trigger an immune response (such as antibody production).
When two flu viruses are antigenically different (i.e., of different subtypes, e.g., H vs. N), a person’s immune response (antibodies) from having one will not develop immunity and protect against the other. However, infection from one H or N virus will help protect against others of the same subtype. Additionally, influenza A(H3N2) viruses also change both genetically and antigenically, and have formed many separate, genetically different clades in recent years that continue to co-circulate.
To combat as many variations as practical, seasonal flu vaccines are formulated to protect against influenza viruses known to cause epidemics, including: one influenza A(H1N1) virus, one influenza A(H3N2) virus, one influenza B/Victoria lineage virus, and one influenza B/Yamagata lineage virus. So, getting a flu vaccine can protect against these viruses as well as additional flu viruses that are antigenically similar.
Overall, influenza A(H3N2) infection is generally more severe than A(H1N1) or B in terms of fever, leukopenia, and C-reactive protein. Myalgia and other symptoms such as fever, headache, general malaise, and sore throat were equally frequent in influenza A(H3N2), A(H1N1), and B infections. Gastrointestinal symptoms were more common in influenza B.
The composition of the U.S. flu vaccine is reviewed and updated annually. The FDA recommendations for this year’s vaccine compositions included updates for H3N2 and B/Victoria, along with continued protection again H1N1 and B/Yamagata. Current data from public health laboratories monitoring the proportion of circulating viruses show 99.9% to be Influenza A, with 77.2% being H3N2 and 22.8% being H1N1, the vaccine is expected to be very protective against the current strains.
COVID Risk Matrix:
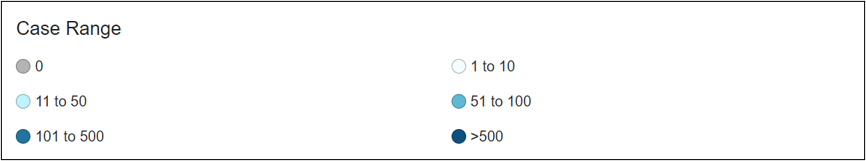
Monkeypox:
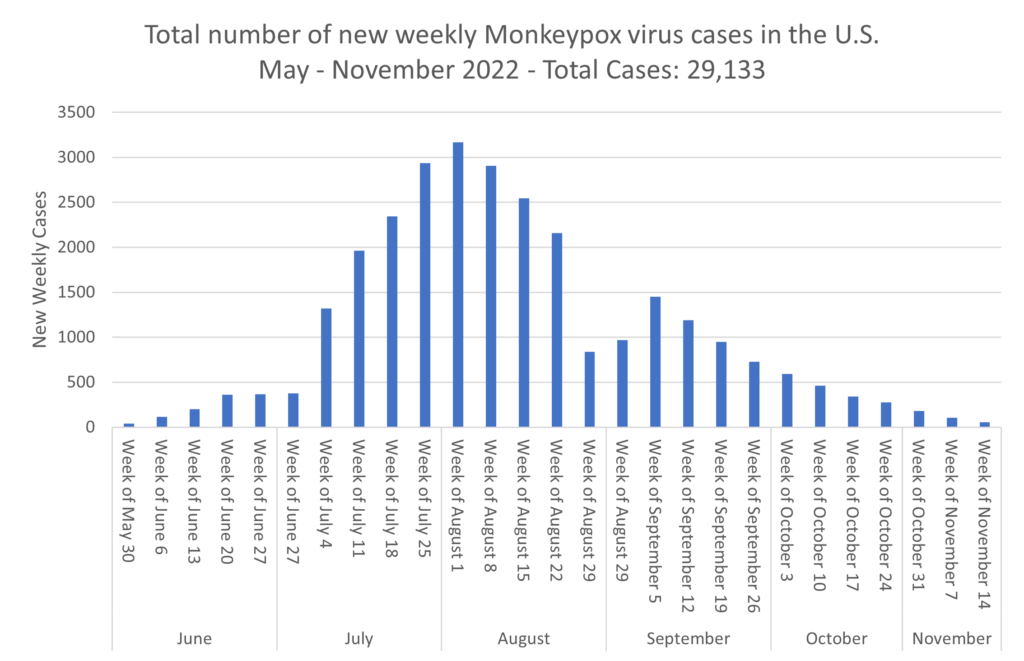
Influenza:
Infectious Disease News
- Shigella. More than 110 people hospitalized as shigella outbreak in Edmonton grows. There are 172 confirmed cases in Edmonton. This first person became ill on August 17, 2022. This could turn into a disaster quickly for the homeless due to the lack of access to bathrooms.
- RSV. Kids are getting hit hard by respiratory viruses. Here’s what scientists know — and what they don’t. Most people tend to catch RSV by the time they are a toddler and with this current wave hitting across North America, there may be a ripple effect from the early days of the COVID pandemic. Social distancing, mask wearing, and widespread lockdowns lead to more individuals working from home, which resulted in many people skipping a year of infections. The immune system’s antibody production after RSV infection drops off fairly quickly. People are more susceptible to infection, antibodies aren’t as prevalent, and mothers who weren’t exposed aren’t transferring as many antibodies to their infant during breast feeding. Adults may also be experiencing lingering debilitating long COVID symptoms, which may be tied to the virus’ impact on immune systems.
- Ebola in Uganda – while some reports seem to indicate a slowing of transmission, there were reports of a case in regions outside of central Uganda, so the outbreak is not over. Vaccine trials will get underway soon. A possible case in the UK is being investigated.
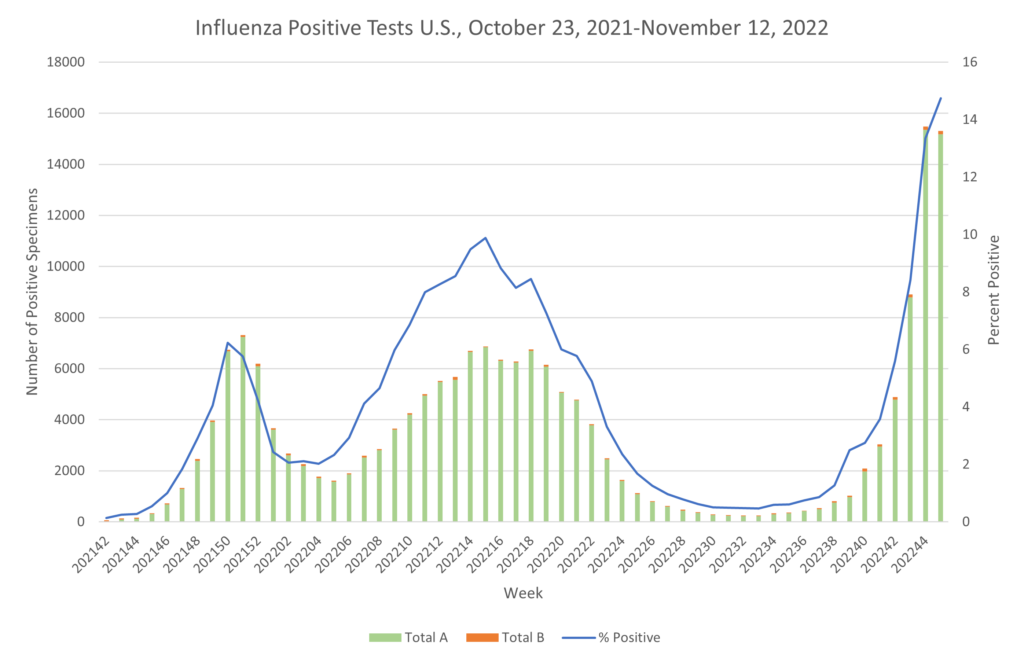
- Influenza. Flu activity continued to rise across the U.S. in the past week, adding to a crunch on emergency departments and pediatric hospitals from an early surge in respiratory viruses. Flu has caused an estimated 4.4 million illnesses, 38,000 hospitalizations and 2,100 deaths so far this season including seven pediatric deaths, the Centers for Disease Control and Prevention said Friday. The highest flu hospitalization rates are among adults ages 65 and older, followed by children under the age of 5, the CDC said. In Canada, at the national level, influenza activity has crossed the seasonal threshold, indicating the start of an influenza epidemic. All surveillance indicators are increasing, and most are above expected levels typical of this time of year. The report cites data from the Centers for Disease Control and Prevention, which showed that five out of every 100,000 people in the U.S. were hospitalized with the flu during the week ending Nov. 5. It’s the highest hospitalization rate this early in the flu season since 2010.
- Measles. During the COVID pandemic, measles cases in India dropped to the lowest in many years, mainly because of COVID restrictions and children staying home. Now with relaxation of COVID restrictions, India has the highest number of cases in the world between April and September 2022.
- TB. Despite being curable, TB remains the world’s oldest and most prevalent infectious disease today. This is because TB is unlike other infectious diseases as it has a long latent period. Infection may not develop into TB disease for months or even years later, and there is no effective vaccine to protect against pulmonary TB, which affects the lungs and is the most common form of TB among adults. Despite there being a vaccine, there are drugs that can be taken to combat the infection, but they may not be widely used. Recent findings from a London study indicate that a considerable fraction of individuals are likely suffering from undiagnosed TB due to the SARS-CoV-2 pandemic and are at an increased risk of disease transmission.
- COVID. Adjusted for population size, the United States had 155,000 to 466,000 more deaths than peer nations in the second half of 2021 and early 2022, the investigators estimated.





