In last week’s article, we discussed indicators that we’re seeing a potential uptick in COVID cases this summer or in the fall. Since the pandemic, the virus has been tracked primarily by case counts and/or hospitalizations, but as research continues about this and other viruses, different tracking methods are coming to the forefront, such as wastewater surveillance. Wastewater-based epidemiology (WBE) is not new, but its use in detecting community levels of SARS-CoV-2 is proving to be a more thorough way of tracking the virus, enabling the detection of asymptomatic and other unreported cases.
For example, new research is showing that WBE can be used to predict county-level hospital admissions with a lead time of 1–4 weeks. As stated by research co-lead by Professor Qilin Wang, “the research shows wastewater surveillance combined with AI-based modeling can be a cost-effective early warning system, allowing public health officials to better prepare for and manage pandemic waves, and efficiently allocate limited healthcare resources.”
Another study notes that the reporting of wastewater surveillance to CDC’s National Wastewater Surveillance System (NWSS) can be used to compare wastewater concentrations with SARS-CoV-2 levels, to enable the evaluation of COVID community changes. This becomes even more important as formal case testing declines.
Such tracking is important to the business world, as it can keep companies informed on evolving levels of COVID and other viruses in their area to help predict and plan for absenteeism before a lack of personnel becomes an issue. In next week’s issue, we will take a look at some of the WBE data trackers to provide more information on how the data is being used and its current status.
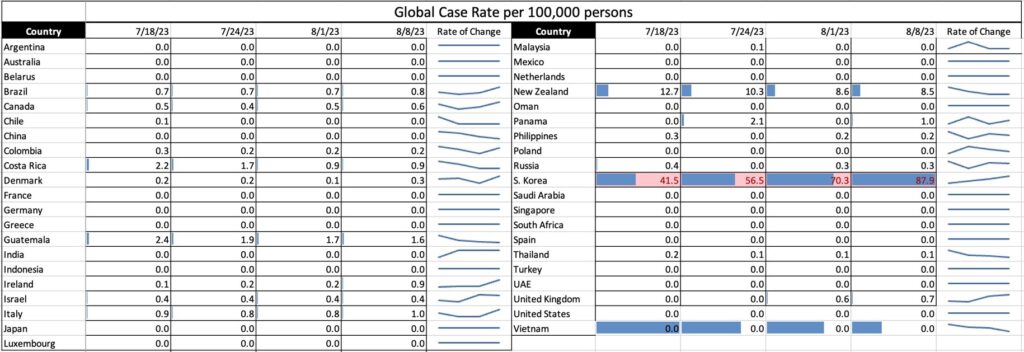
COVID Risk Matrix:
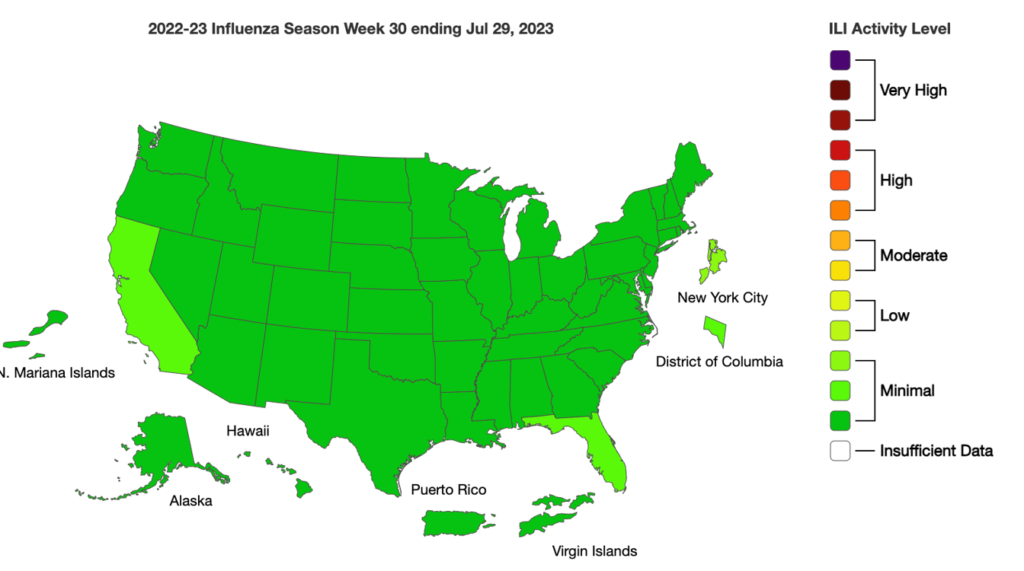
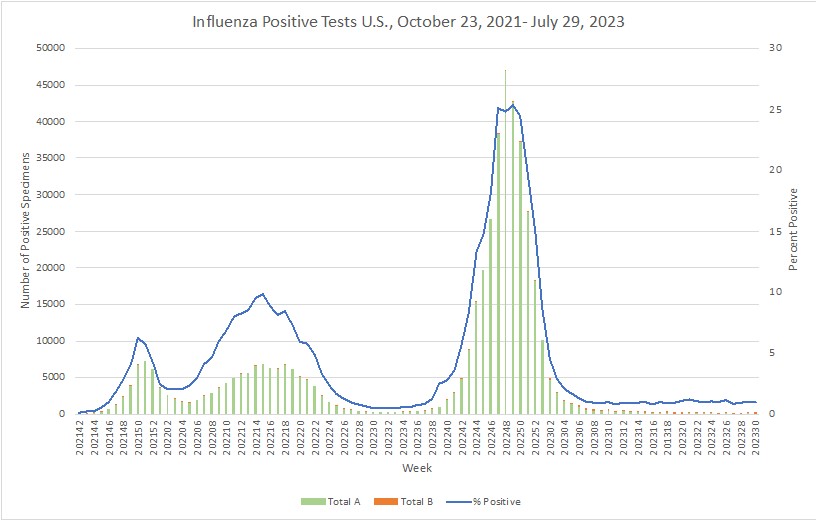
Influenza:
- With the aging population in China, the incidence of Shingles is increasing, and mainly targeting middle-aged and elderly people. It is estimated that 1.56 million new cases of herpes zoster occur each year among people aged 50 and over in China. Vaccinations are available and educational campaigns are being stepped up to encourage their uptake.
- Respiratory viruses that were suppressed through previous lockdowns during the COVID-19 pandemic have recently started to co-circulate with SARS-CoV-2. This study describes and compares the proportion of symptoms reported during illnesses infected by common respiratory viruses. The SARS-CoV-2 symptom profile increasingly resembles that of other respiratory viruses as new strains emerge. Increased cough, sore throat, runny nose, and sneezing are associated with the emergence of the Omicron strains. As SARS-CoV-2 becomes endemic, monitoring the evolution of its symptomatology associated with new variants will be critical for clinical surveillance.
- A recent study showed that antibiotic use during the COVID pandemic was increased throughout the US, and other parts of the world. Specifically, there was a large increase in azithromycin, which probably is reflective of the fact that many doctors believed it could be used to treat COVID.
- CDC reported 2023’s first two human infections of swine flu. The infections occurred in individuals who attended different agricultural fairs in Michigan and had contact with pigs. To date, no person-to-person spread of this virus has been identified.
- By the end of week 30, 2023, stable trends were observed in all EU/EEA indicators. Among the EU/EEA countries reporting cases of COVID-19, five showed an increase in overall case rates compared to the previous week. These increases were recent (of 1–2 weeks duration) and the indicators remained relatively low, compared with pandemic peaks. There were 50 deaths reported from 14 countries.
- EG.5, the latest Omicron subvariant, has been circulating the world. Experts have said this subvariant appears to be more infectious and able to sneak past immune defenses, but there isn’t much evidence to suggest it causes more severe illness.





