Studies are showing that untreated, raw milk containing the H5N1 virus poses a high risk of infection in susceptible animals. With heat inactivation/pasteurization showing efficacy in killing the virus, TAG highly recommends against the consumption of raw milk.
In a recent study published in the New England Journal of Medicine, researchers from the University of Wisconsin-Madison and Texas A&M Veterinary Medical Diagnostic Laboratory studied the effect of H5N1-contaminated raw milk on mice. Samples were taken from cows in New Mexico, who were infected with eight isolates, all within the same clade, of the HPAI A (H5N1) virus.
Five mice were given 20 drops of the milk each and exhibited immediate symptoms of infection (ruffled fur and lethargy) on day 1. On day 4, the mice were euthanized and examined. Findings showed high levels of avian flu in the mice’s respiratory tissues, including nasal passages, trachea, and lungs. Low-to-moderate levels of the virus were found in other tissues. In two of the mice, the virus was found in the mammary glands, which has been seen in cows as well.
This study looked at the effects of time and temperature on virus inactivation, with pasteurization showing efficacy in inactivating H5N1 molecularly in milk. The results showed that heating the raw milk to 145°F successfully inactivated the virus at intervals of 5, 10, 20, and 30 minutes. When the milk was heated at 161.6°F but for shorter periods of time (15 and 20 seconds), the virus was still viable but viral load did decrease. Longer pasteurization times are needed because the fat molecules and casein micelles in milk surround and protect the virus from inactivation. Storage of influenza-contaminated raw milk at 39.2°F for 5 weeks only slightly decreased H5N1 virus levels, showing that the virus is infectious in refrigerated milk for several weeks.
Researchers suggest cows could be “an influenza mixing vessel” after analyzing cow tissues. A team of scientists from the University of Copenhagen and St. Jude’s Children’s Research Hospital in Memphis, Tennessee found duck and human-type influenza A receptors in the dairy cow’s mammary glands and chicken-type influenza receptors in the cow’s respiratory tract. This finding suggests cows may act as hosts of infection and evolution of both the avian flu and human influenza viruses.
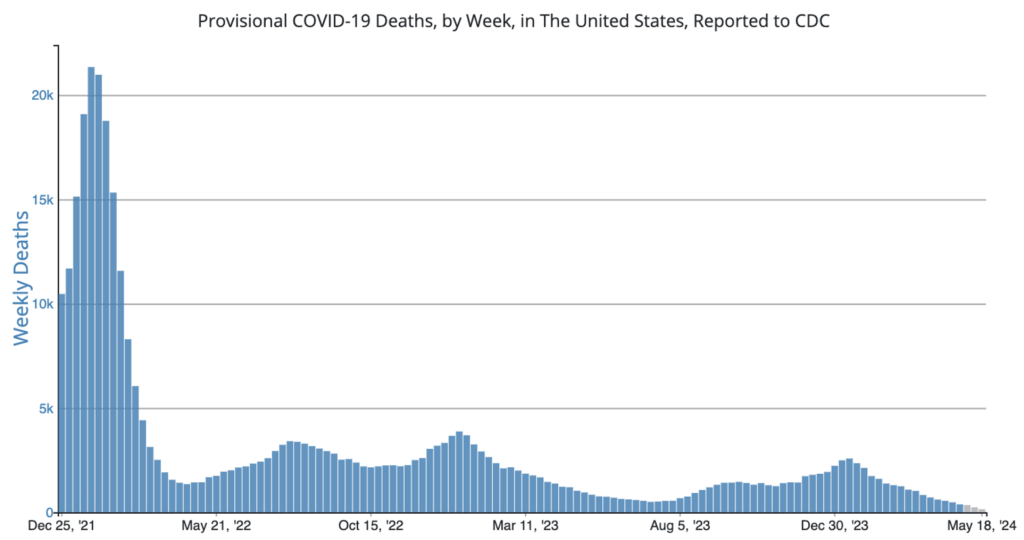
COVID Risk Matrix:
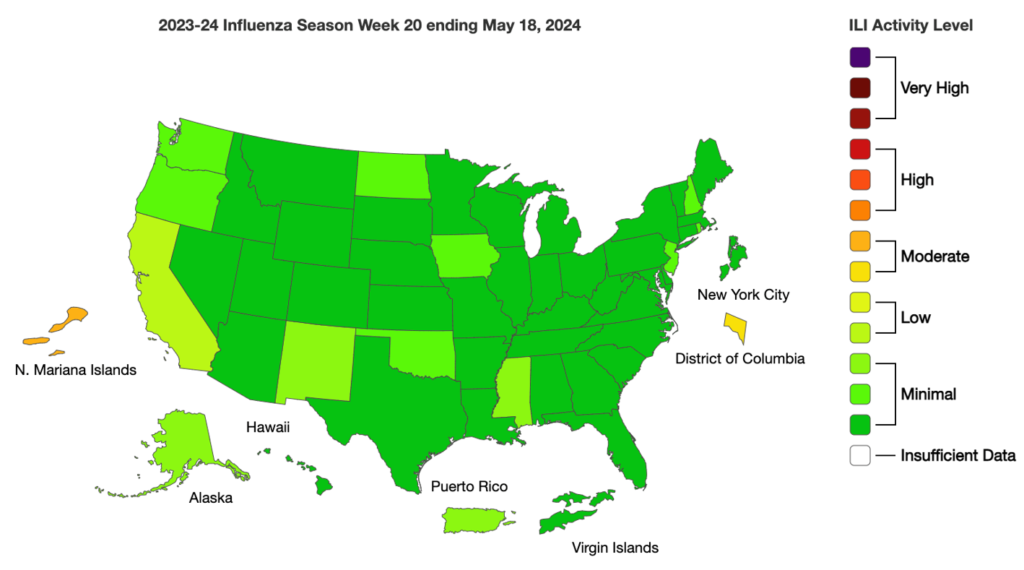
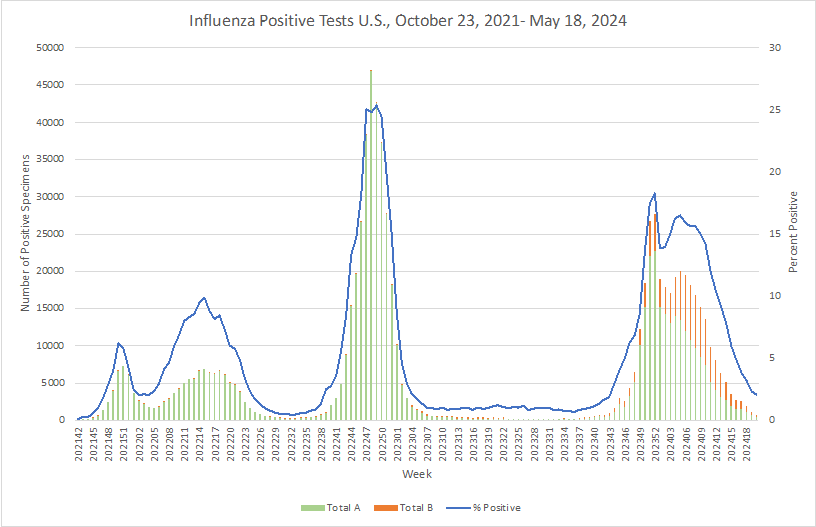
Influenza:
- The US CDC has issued a travel notice related to risks of meningococcal disease associated with travel to Mecca June 14-19, 2024. 12 cases have been linked to travel in the area since April 2024.
- The FDA is continuing to advise consumers not to eat and restaurants and food retailers not to serve or sell and to dispose of frozen, raw, half-shell oysters processed by JBR (KR 15 SP) in Tongyeongsi, Republic of Korea on Nov. 27, 2023, Jan. 4, 2024, and Feb. 15, 2024, and shipped to distributors in California because they may be contaminated with norovirus.
- UKHSA figures show 91.6% of babies in the UK had received vaccinations by their first birthday, which provides immunization against a range of diseases including whooping cough. It’s recommended that 95% of babies receive such vaccinations for protection.
- Cases of hepatitis and gastroenteritis are increasing in Mumbai, likely due to the consumption of contaminated water.
- Four alpacas have become infected with H5N1 avian flu in Idaho as reported this week by the USDA. The virus had struck a poultry flock on the farm prior. These positive tests are the first findings in alpacas.
- China reported its first fatality associated with H5N6 avian flu. The individual was a 52-year-old woman. The woman’s symptoms began on April 13, she was hospitalized on April 20, and she died on April 30. She had been exposed to backyard poultry before becoming ill.





