With Hepatitis A in the news the last few weeks with local outbreaks reported in Georgia, Maine, and Massachusetts, TAG has had clients asking about worker vaccination, particularly in locations that mandate Hep A vaccines for food workers. While outbreaks most commonly stem from foodservice, there’s no shortage of cases linked to fresh fruits and vegetables, both domestic and foreign.
There is only a shortlist of jurisdictions, such Franklin and St. Louis counties in Missouri, that mandate vaccines for certain foodservice workers, but some jurisdictions do not allow unvaccinated workers to work if the establishment is in an outbreak situation. Additionally, due to the serious nature of the virus, Hepatitis A is a reportable illness, and most public health departments highly recommend that all workers at establishments where a hep A outbreak occurs be vaccinated.
Hepatitis A vaccines were first licensed for use in the United States in 1995; in 1996, vaccinations were advised for children living in communities with high rates of infection and disease. Currently the CDC recommends that all children get the hepatitis A vaccine between 12 and 23 months of age, as well as those up to 18 years of age who have not been vaccinated. Additionally, more than half the states in the U.S. have Hep A vaccine requirements for children in childcare and/or school, with the U.S. Supreme Court upholding states’ authority to require vaccination to protect public health and safety. Even with this, however, there is a group of persons who work in foodservice who were born before the Hep A vaccine was placed on the regular schedule, or attended school in a state that does not require the vaccine for schoolchildren. It is this group that is of potential concern today.
So, when and why should you encourage your workers to be vaccinated?
- If you are in one of the few jurisdictions requiring vaccination, you don’t have much choice. As specified in the St. Louis County Food Code, a person cannot be employed as a food handler for more than 30 days unless and until written certification by a health care provider verifies that the person is immune from, or has been vaccinated against, Hepatitis A. So, this verification should be requested upon hire, or the person given 30 days to provide it.
- If your food establishment is within the current outbreak area, encourage employees to get vaccinated. Explaining why this is important can help with compliance. Being in proximity to an outbreak increases one’s chances of being infected, and a single dose of single-antigen hepatitis A vaccine has been shown to successfully control outbreaks, as it is effective even after exposure. While most people successfully recover from symptoms, acute hepatitis can lead to liver failure and death.
- The vaccine is available through most healthcare providers and pharmacies. Those without health insurance coverage should contact the local health department to check on the availability of free or low-cost vaccinations.
Additionally, to reduce the chance of transmission in your food facility,
- Instruct employees to report any illness symptoms – especially jaundice (yellow skin) – and inform you immediately if a household member, or other close contact, has been diagnosed with HAV.
- If you have an infected worker, send the worker home immediately; notify your local health department; and request guidance on what to do and when the employee can return to work.
- Ensure that effective handwashing protocols are in place and fully implemented by all employees. Guidance from the US Food Code in section 2-3 “Personal Cleanliness” outlines when handwashing should be done and how to wash.
For more information on Hepatitis A, see TAG’s Infectious Disease Fact Sheet, and contact us for assistance.
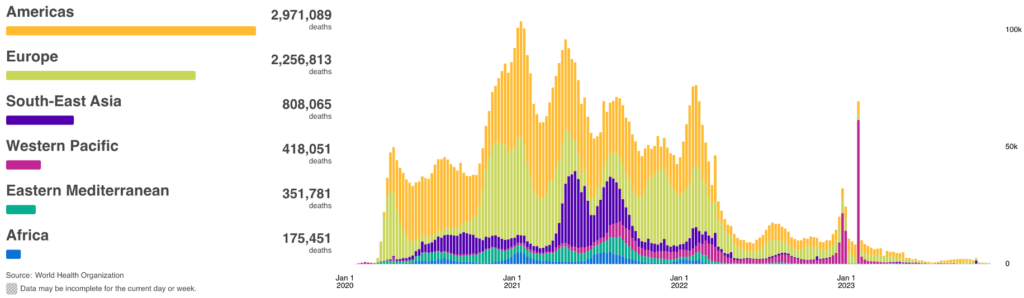
COVID Risk Matrix:
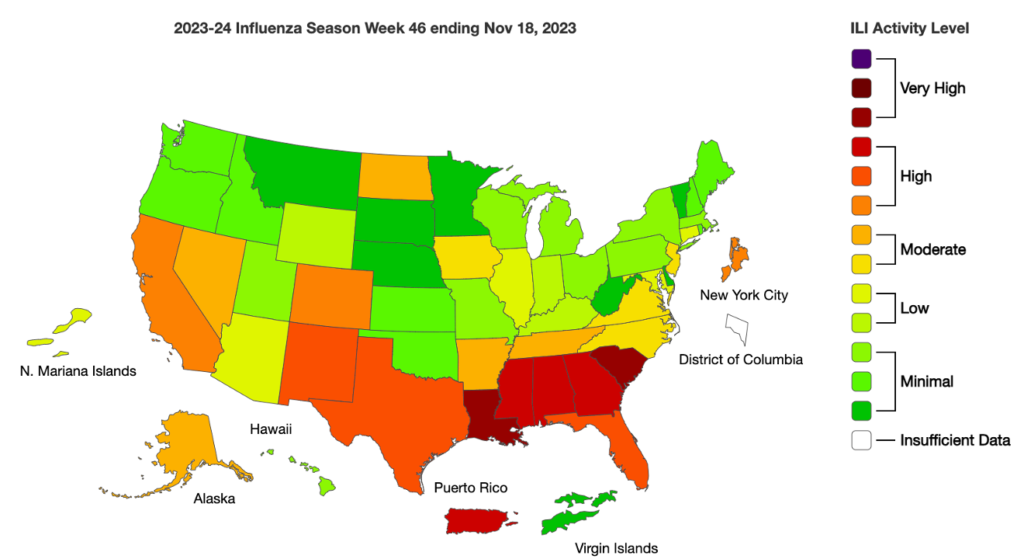
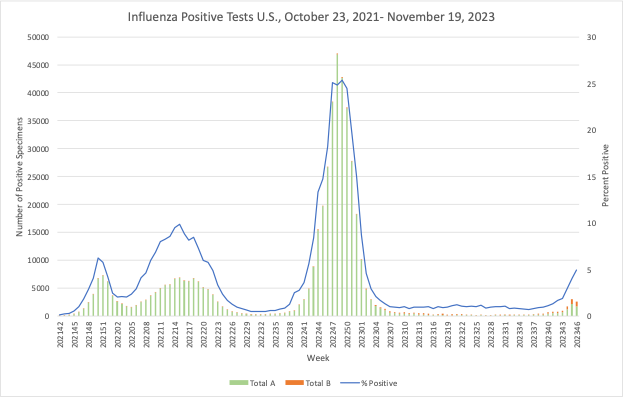
Influenza:
Infectious Disease News:
- Canada’s daycare kitchen that was found at the center of the E. coli outbreak this year has now reopened on a limited basis. The kitchen is only allowed to serve one of the 11 daycare centers that were closed due to the illnesses. It was discovered that meatloaf and veggie loaf made at the central kitchen was the source of the outbreak.
- A CDC study showed that influenza vaccination coverage among health care personnel in acute care hospitals declined after the COVID-19 pandemic from an average rate of 85% to about 81%. Rates were lower in rural areas and among contract employees. Another reason for the decrease may be due to more emphasis being placed on COVID vaccines and less on the importance of flu vaccines.
- Cardiff has the most suspected cases of measles anywhere in England and Wales.
- The Evanston, IL Health and Human Services Department is investigating a norovirus outbreak linked to a $1-burrito November 18, event for Northwestern University students. Cleaning and sanitizing is occurring at the establishment that prepared the food, though the link to this restaurant has not been confirmed.
- RSV is on the rise, specifically being recognized in Canada. RSV cases are currently above expected levels for this time of year, claims the Public Health Agency of Canada. Cases of RSV have a 5.3% positive rate while influenza is recording a 4.3% positive rate throughout Canada.
- Health Canada has granted approval to lift a ban on blood donations from people who lived or traveled in the UK, Ireland, or France for long periods of time in the 1980s and 1990s. Individuals that fell into these criteria will be eligible to donate blood on December 4.





