Continuing federal studies are finding that food safety practices will kill avian influenza in foods, with USDA experiments showing H5N1 to be killed through the proper cooking of ground beef and FDA research finding pasteurization to be effective in killing the virus in milk.
- The USDA experiment found that no virus was found when the beef, inoculated with high levels of an H5N1 surrogate virus, was cooked to an internal temperature of 145°F (medium) or 160°F (well done). However, the virus was still present, at reduced levels, when only cooked to 120°F (rare). USDA continues to advise that ground beef be consumed only when cooked to a temperature of 160°F.
- In follow up to the FDA May 10 announcement that all samples (297) from an initial retail dairy product survey were negative for H5N1, the agency provided further updates on May 20 based on pasteurized milk samples collected at retail locations in 17 states and analyzed through USDA-ARS qRT-PCR screening. While some of the samples were shown to contain H5N1 viral nucleic acid, none of these were positive for the live virus – proving the effectiveness of pasteurization.
- The agencies are continuing their studies; however, USDA has had difficulty finding affected dairy farm workers willing to be tested, despite a $75 incentive.
CDC is also continuing its work in H5N1 studies, as it will be developing greater surveillance of H5N1 outbreaks in dairy herds this summer through increased testing. The Center also has started using the Influenza Risk Assessment Tool (IRAT) to assess the H5N1 virus and is continuing to monitor wastewater for influenza A and conduct intensive surveillance reviews at sites with high levels of detection.
Although the multi-state outbreak among dairy cattle is ongoing, as of May 21, CDC is reporting only two human H5N1 cases in the U.S. (since 2022) with no person-to-person spread. Thus, CDC continues to state that the current public health risk is low.
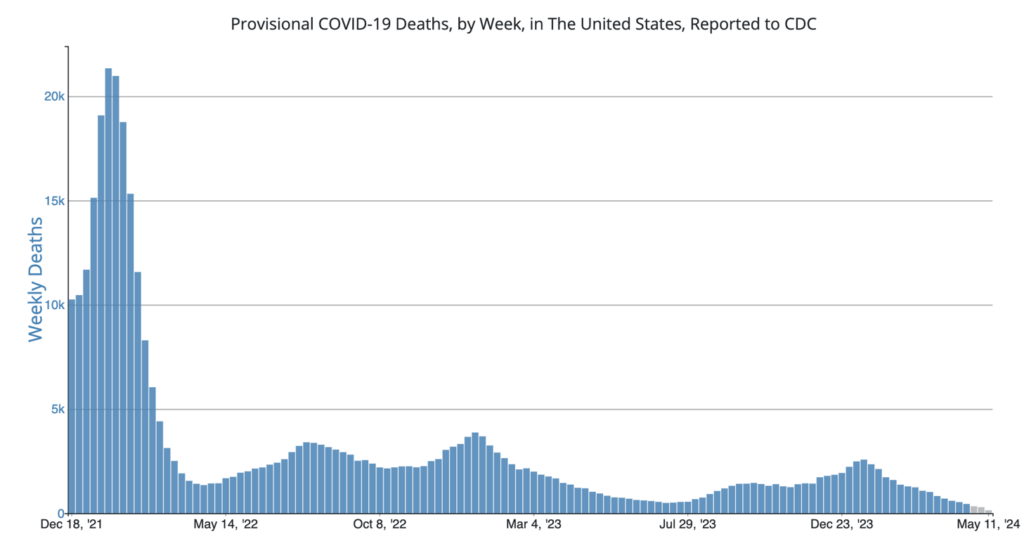
COVID Risk Matrix:
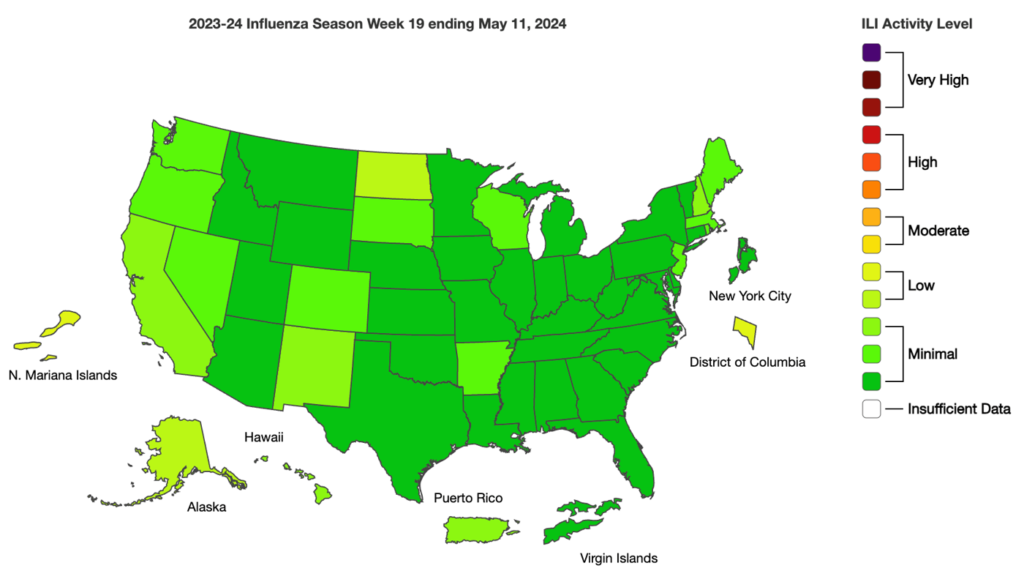
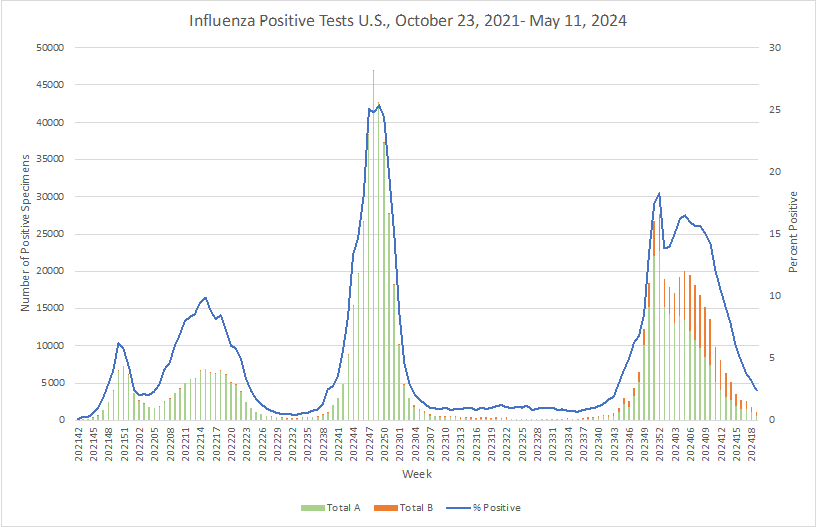
Influenza:
- The final report of the U.K.’s infected blood inquiry, published nearly six years after its inception, reveals that tens of thousands contracted HIV or hepatitis from tainted blood transfusions in the 1970s and 1980s, leading to around 3,000 deaths. The report criticizes medical practitioners, civil servants, and politicians, and suggests a substantial compensation bill for the British government. Campaigners, like Jason Evans, whose father died from infected blood, were pivotal in bringing the scandal to light and initiating the inquiry. The findings highlight missed opportunities to prevent contamination and underscore the need for accountability and compensation.
- Avian influenza has been detected in three more dairy herds in Michigan. These new counts bring the total detection to 18 herds throughout Michigan. H5N1 has been detected in two domestic cats in South Dakota, neither of them contracting the virus from affected poultry farms or dairy farms.
- USDA experiments suggest H5N1 is not viable in properly cooked ground beef.
- The US Centers for Disease Control and Prevention (CDC) on May 20, 2024, issued a health alert and a level 1 travel alert about meningococcal disease in travelers to Saudi Arabia, especially those taking part in pilgrimage activities.
- The World Health Organization (WHO) on May 17, 2024 updated its list of the bacterial pathogens it considers to be the biggest threat to human health. Primary focus is on pathogens known to be resistant to antibiotics. The WHO reports, “The 2024 WHO BPPL covers 24 pathogens, spanning 15 families of antibiotic-resistant bacterial pathogens. Notable among these are Gram-negative bacteria resistant to last-resort antibiotics, drug-resistant mycobacterium tuberculosis, and other high-burden resistant pathogens such as Salmonella, Shigella, Neisseria gonorrhoeae, Pseudomonas aeruginosa, and Staphylococcus aureus.”
- The World Health Organization (WHO) announced that it has prequalified a second dengue vaccine, TAK-003, known as Qdenga and developed by Takeda.
- In April 2024, the UK Health Security Agency is reporting norovirus cases at rates 75% above the 5 year average for the same 4 week period.





